Review
Diagnostic deadlock: A Case of Disseminated Tuberculosis with Neuroleptospirosis
Diagnostic deadlock: A Case of Disseminated Tuberculosis with Neuroleptospirosis
Sanchit Shailendra Chouksey1a, Pranjali Batra2 a, Rameshwar Nath Chaurasia3a, Pratistha Sengar4b, Varun Kumar Singha*
Varun Kumar Singh, M.D., D.M., Associate Professor, Department of Neurology
Institute of Medical Science, Banaras Hindu University, Varanasi-221005,
Email: mailurvarun@gmail.com
Abstract:
Neuroleptospirosis may present with altered sensorium, generalised tonic clonic seizures, headache, and focal neurological deficit. Common neurological manifestations of tuberculosis include meningitis, tuberculoma and arachnoiditis. We report a case of a young male who presented with features of acute meningoencephalitis. Serum IgM leptospira titer was high and blood PCR was positive for leptospira. Patient received ceftriaxone and doxycycline for two weeks. There was improvement in sensorium, however high-grade fever persisted. On further evaluation, he was also found to have disseminated tuberculosis. He was started on anti-tubercular therapy. Later he developed refractory status epilepticus and succumbed to illness. This is a rare case report of coexistent neuroleptospirosis and disseminated tuberculosis creating diagnostic and therapeutic dilemma. The case also emphasises the importance of revising one’s own diagnosis and further work up once the anticipated therapeutic response is inadequate.
Keywords: Neuroleptospirosis, Tubercular Meningitis, Pott’s spine, Refractory Seizure
Introduction:
Leptospirosis is the most prevalent zoonosis in the world. [1] The neurological manifestations of leptospirosis include meningitis, encephalitis, intracranial bleed, cerebellitis, movement disorders, myelitis , flaccid paraparesis, mononeuritis, autonomic lability and polymyositis.[2] Tuberculosis most commonly affects lungs, however the involvement of central nervous system carries more morbidity and mortality.[3] Here we describe a case of a young male who presented with features of acute meningoencephalitis, initially diagnosed as neuroleptospirosis, later also found to have disseminated tuberculosis leading to initial diagnostic dilemma.
Case report:
A 19-year-old male presented with high-grade fever, holocranial headache and projectile vomiting for 4 days and right focal to bilateral tonic clonic seizures associated with loss of consciousness for 3 days. There was no history of cough, myalgia, jaundice, reduced urine output or bleeding manifestations. His birth and developmental history were normal. Past history was also non-significant.
On examination, he was febrile (101°F), and respiratory rate was 22 breaths per minute. Rest of general physical examination, cardiovascular and abdominal examinations were within normal limits. Chest examination revealed coarse crepitations in bilateral lung fields. On neurological examination, his Glasgow coma scale (GCS) score was E2V1M5. There was no papilledema. He was moving all four limbs to painful stimuli. Plantar response was bilateral extensor. Signs of meningeal irritation were present. Cranium and spine were normal. A provisional diagnosis of acute meningoencephalitis was made.
Patient was started empirically on ceftriaxone 2 grams twice daily, acyclovir 500 mg thrice daily, artesunate 2.4 mg/kg stat followed by 2.4 mg/kg at 12 and 24 hours and doxycycline 200 mg stat followed by 100 mg twice daily. For seizure, he was given lorazepam and levetiracetam initially. Refractoriness led to sequential addition of other antiepileptic drugs (levetiracetam 1.5 gm twice daily, valproic acid 1 gm twice daily and lacosamide 200 mg twice daily). He was intubated and started on midazolam infusion at 0.2 mg/kg/hour leading to subsidence of seizure. He was extubated on day 7.
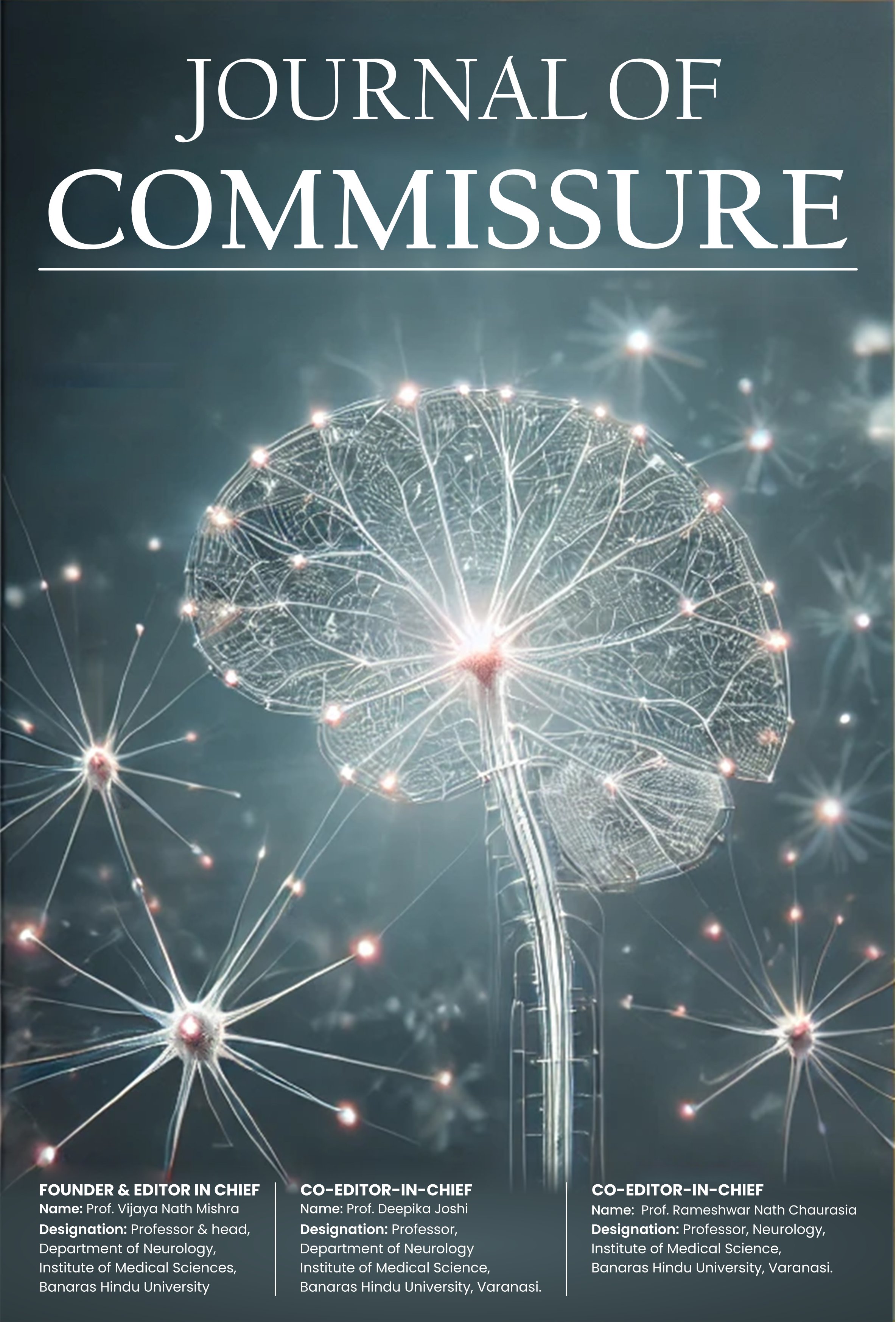
His initial laboratory data normal complete blood count, but elevated alanine transaminase 74 U/L (10-40 U/L), aspartate transaminase 45 (10-40 U/L), and creatine kinase 493 U/L (24-195 U/L). Serology for hepatitis B, C, and human immunodeficiency virus (HIV) were negative. Cerebrospinal fluid (CSF) showed a raised pressure of 40 cm of water, cell count 280 cells/µL (Neutrophils-15%, Lymphocytes- 85%), protein 149 mg/dL, glucose 12 mg/dL (corresponding blood sugar 98 mg/dL) and no bacterial or fungal growth. CSF cartridge-based nucleic acid amplification test (CBNAAT) and viral panel reports came negative. Serum immunoglobulin M leptospira titer was 26.4 Units (<9 units). His blood polymerase chain reaction (PCR) was also positive for leptospira. By day 9, there was an improvement in sensorium. However, the fever did not subside despite 2 weeks of doxycycline therapy. He also started complaining of low back ache with tenderness over lumbar spine. Contrast-enhanced computed tomography (CECT) thorax, abdomen and pelvis was suggestive of disseminated tuberculosis (Fig. 1).
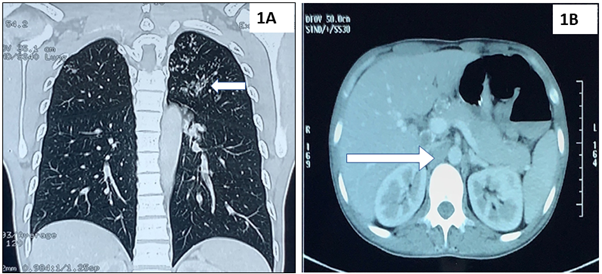
Fig. 1: Contrast enhanced computed tomography of chest and abdomen revealing multiple centrilobular nodules in upper lobe of left lung parenchyma (1A) and multiple enlarged mediastinal, bilateral hilar and intraabdominal (arrow) lymph nodes (1B) suggestive of disseminated tuberculosis.
He was started on 4 drugs antitubercular therapy. His magnetic resonance imaging (MRI) brain and spine with contrast revealed diffuse leptomeningeal enhancement and basal exudates with hydrocephalus and lytic lesion at L4 vertebrae suggestive of tuberculous meningitis and Pott’s spine (Fig. 2).
Fig. 2 Contrast magnetic resonance imaging of brain showing leptomeningeal enhancement and basal exudates on T1W (2A) and hydrocephalus on T2W with periventricular ooze (2B) suggestive of tuberculous meningitis. Contrast magnetic resonance imaging of lumbosacral spine, T1W sagittal and axial images, revealing ill-defined lytic-permeative lesion in L4 vertebral body (2C) with associated soft tissue density thickening in prevertebral space along anterior longitudinal ligament and posteriorly extending into intradural compartment (2D) suggestive of Pott’s spine.
Ventriculoperitoneal (VP) shunting was done. He had further improvement in sensorium in post-operative period with CT head showing reduction in hydrocephalus (Fig. 3). 
Fig. 3 Axial computed tomography of head (Post operative day 5) showing in situ ventriculoperitoneal shunt with complete reduction of the hydrocephalus.
However, he again developed status epilepticus despite of ongoing antiepileptic drugs on post operative day 10. He was put on mechanical ventilator. He further developed ventilator associated pneumonia and succumbed to the illness.
Discussion: The present case was a young male who presented with fever, headache, vomiting and refractory seizures. He was found to be positive for IgM leptospira. Blood PCR was also positive for leptospira. The recommended treatment of was given for fourteen days. However, fever was persistent. A detailed evaluation revealed disseminated tuberculosis in lungs, spine, abdomen and brain. He underwent ventriculoperitoneal shunt for hydrocephalus. However, he succumbed to the refractory seizure and septic shock later in the hospital course.
Leptospirosis is a worldwide zoonotic disease caused by a spirochete Leptospira interrogans. Neuroleptospirosis has been reported in 11.6% of patients of leptospirosis. The CNS manifestations include headache (37.2%), altered sensorium (38.4%), meningism (7%), generalised tonic clonic seizures (3.5%), focal neurological deficit (2.3%).[4] Neuroleptospirosis carries good prognosis if the treatment is initiated in the earlier course of disease, however, seizures and altered sensorium portend worse prognosis in neuroleptospirosis.[2] In the present case, both these bad prognostic factors were present.
Central nervous system (CNS) manifestations represent the most debilitating infection of Mycobacteria tuberculosis. It may present as tuberculoma, tubercular meningitis (TBM), tubercular abscess or arachnoiditis.[5] Poor prognostic indicators include advanced age, disseminated tuberculosis, low GCS score at the time of admission and hydrocephalus. The prevalence of seizures in patients with TBM is about 34%. Early onset seizures in tuberculosis are associated with meningitis and late onset seizures are associated with tuberculoma, infarction and hyponatremia. [6] In a study, the frequency of seizures reported was 20.6% where single episode of seizure was noted in 30.4%, repetitive seizures in 54.3% and status epilepticus in 15.2% and mortality was observed in 34.8% of patients with seizures. [7] Low GCS score, hydrocephalus, disseminated tuberculosis and refractory seizure were present in above case.
In present case, neuroleptospirosis was thought initially as an aetiology for acute meningoencephalitis. However, persistence of fever despite of the full course of standard therapy of leptospirosis led to suspicion of either coexistent other disease or false positivity of IgM leptospira owing to cross reactivity. A homologue of mammalian cell entry (Mce) protein, normally found in Mycobacterium tuberculosis, is also present in pathogenic leptospira species that may explain the cross reactivity.[8] However, in present case high titer of IgM leptospira, positive PCR, deranged liver enzymes and elevated creatine kinase levels support the co-existence of leptospirosis and tuberculosis.
Conclusion: This is a rare case report of coexistent neuroleptospirosis and disseminated tuberculosis creating diagnostic and therapeutic dilemma. This case also highlights the importance of revising the diagnosis and further work up once the anticipated therapeutic response is inadequate in a particular disease entity.
References:
|
|
|
|
|